Checkpoint inhibitor therapy
A form of cancer immunotherapy targeting immune checkpoints, which are key regulators of the immune system that, when stimulated, can dampen the immune response.
Immunotherapy using “checkpoint inhibitors” (see fact box) is an emerging form of cancer care that is reshaping the role of medical imaging in cancer diagnosis and treatment follow-up. The use of immunotherapy is increasing fast, placing new demands on radiologists to utilize advanced medical imaging techniques and modalities to assess complicated treatment response patterns.
One example of this is how medical imaging must support radiologists in managing the latest relevant response criteria, such as iRECIST. Another example is identifying pseudoprogression, and distinguishing it from hyperprogression, and the detection of adverse events.
This article describes some of these new requirements imposed by immunotherapy and how medical imaging can facilitate radiologists’ diagnosis.
A form of cancer immunotherapy targeting immune checkpoints, which are key regulators of the immune system that, when stimulated, can dampen the immune response.
Some cancers can protect themselves from attack by stimulating immune checkpoint targets. Checkpoint therapy can block inhibitory checkpoints and restore immune system function.[1]
Imaging has been the common language for tumor response assessment for a long time. Advances in cancer therapy are achieved through continual investigation and evaluation of treatment results and their incorporation in the practice of oncology.
Before the age of immunotherapy, cytotoxic agents were the standard of care. Cytotoxic agents directly kill tumor cells and prevent them from growing. An early increase in tumor burden and/or an early increase in tumor size signifies a progressive disease—a scenario where drug cessation is recommended.
Based on the need for a standardized method for describing the results of cancer treatment, the RECIST (Response Evaluation Criteria in Solid Tumors)[2] standard was introduced in 2000, and has since been upgraded several times. RECIST can be seen as a set of published rules that define when tumors in cancer patients improve (“respond”), stay the same (“stabilize”), or get worse (“progress”) during treatment.
The RECIST 1.0 standard included four categories of response to describe treatment progression:
For example, PR according to RECIST 1.0 was defined as a >30% decrease in the sum of target lesion. PD was defined as a >20% increase of the sum of target lesion, or the appearance of new lesions, or unequivocal progression of non-target lesions. A new revision of the standard, RECIST 1.1, was released in 2009.[3]
With the rapid introduction of immunotherapies over the past decade, anti-tumor response may take longer as compared to cytotoxic agent response, and durable stable disease may represent anti-tumor activity. This entails a need for a longer follow-up time to verify “clinically insignificant” progressive disease (PD).
In general, the tumor response to immunotherapy can be described according to four patterns, some of which differ from the traditional response to cytotoxic chemotherapy. These are illustrated in Figure 1 showing the change in tumor size and, in some cases, the introduction of new metastasis (inspiration by Wochok et al., 2009).[3]
A. Decrease in size of tumor. This is the traditional CR or PR response.
B. Stable disease, followed by a slow reduction in overall tumor burden.
C. Initial increase in size of tumor before demonstrating treatment response.
D. Appearance of new lesions after treatment initiation, followed by treatment response.
A clinical response to immunotherapies can, for example, initially manifest conventional progressive disease (PD). This is called pseudoprogression and could mean a treatment response after an identified increase in tumor burden or tumor size, or a response during or after the appearance of new lesions (see Figure 2).
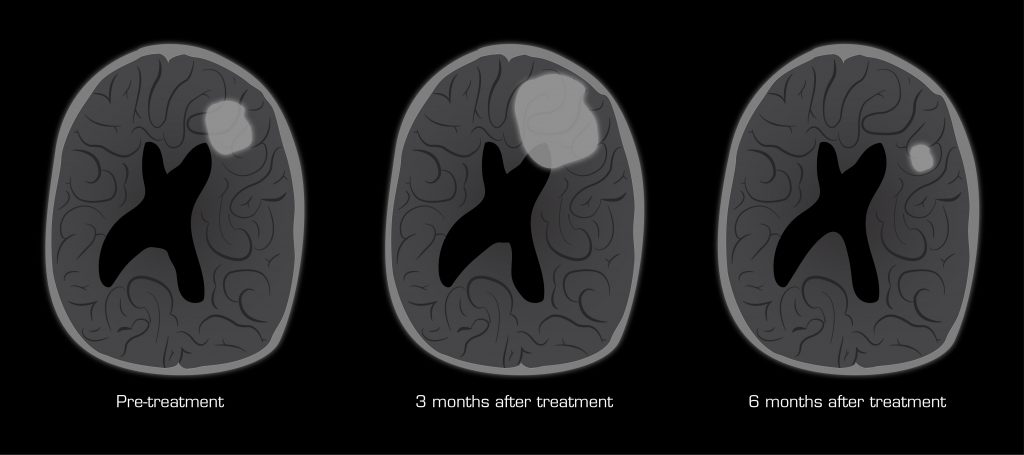
Figure 2. Illustration of consecutive scans showing pseudoprogression as a response to immunotherapy.
Pseudoprogression has a reported incidence of 7% in melanoma, and much lower rates (1.5–3%) in epithelial malignancies[4]. Explanations for pseudoprogression are either a transient infiltration of the tumor with immune cells, accounting for the increase in size on imaging, or the tumor may actually undergo continued growth until the immune system is sufficiently augmented to initiate tumor destruction.
Figure 3 illustrates an example of the tumor burden dynamics in three melanoma cases treated with a PD-1 inhibitor. It shows how the tumor initially grows, and later decreases in size to reach partial response.
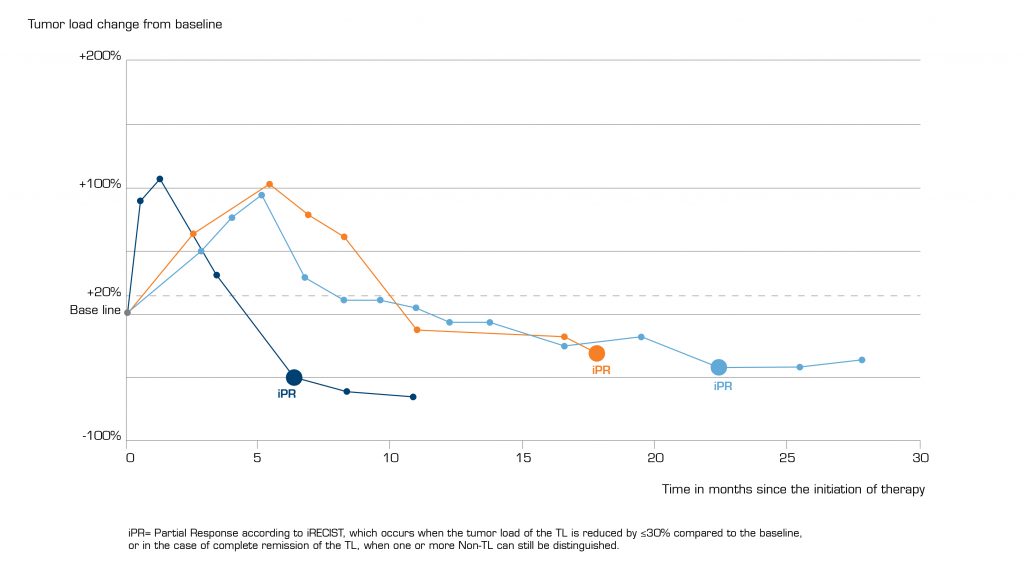
Figure 3. Tumor progression in melonoma cases treated with PD-1 inhibitor. Showing tumor burden in pseudoprogression. The graph has been made with inspiration from Nishino M, et al., 2017[5].
Another phenomenon of immunotherapies is the possibility of accelerating disease progression. Increasingly, cases of so-called hyperprogressive disease (HPD) in patients treated with immune checkpoint inhibitors in multiple disease types have been described. Across various studies, the incidence of HPD among immunotherapy cases ranges from 10–30%.[6]
Treatment with immunotherapy should be stopped early in cases where there is a suspicion of HPD and be replaced by traditional treatments such as chemotherapy. The figure below demonstrates a case of HPD on a patient given immunotherapy and when chemotherapy was used.[6]
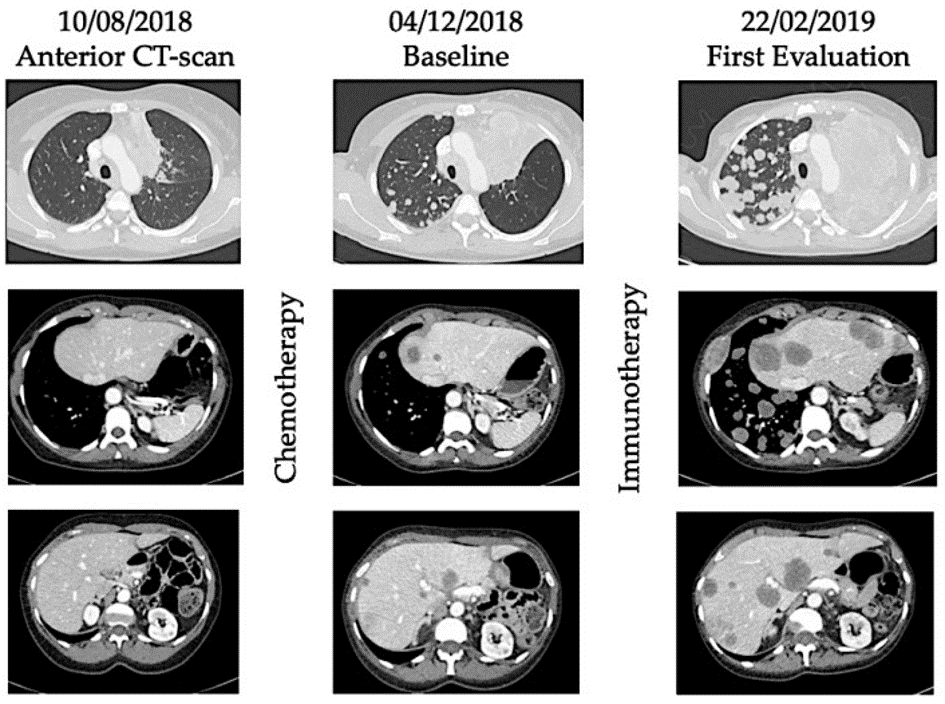
Figure 4. Illustration of hyperprogression under immunotherapy. A 53-year-old female patient with metastatic (lung) submandibular gland epidermoid carcinoma was treated in third line with weekly Methotrexate. After four months, the patient experienced disease progression with the appearance of lung, hepatic and bone metastases. As fourth line, she received Nivolumab, an anti-PD-1 inhibitor. After four injections, she presented with major dyspnea with massive disease progression on a computed-tomography (CT) scan. She died 64 days after immunotherapy initiation. (Thanks to [6] with permission.)
Imaging also plays an important role in detecting immune-related adverse events, which may be caused by the stimulation of the immune system. These events clinically manifest as autoimmune type processes, and can affect many organ systems, most commonly skin, endocrine, gastrointestinal, and respiratory systems, many of which are detectable radiologically. In some cases, the radiological appearance of immune-related adverse effects can mimic disease progression and/or treatment response. Studies have shown that up to 80% of patients receiving immune checkpoint inhibitors such as anti PD-1 or anti PD-L1 experience adverse events.[7]
Adverse events can cause pitfalls is response assessment and using the right imaging modalities, knowledge of symptomatology and imaging patterns are key to detecting adverse events. For example, using PET is better in most cases than CT for early diagnosis of adverse events[8].
Diarrhea is one example of a common symptom in patients receiving immunotherapy, present in up to 45% of patients, with CT evidence of colitis present in 5%.
Pneumonitis is another example of an adverse event that can be seen in up to 5% of patients and in severe cases can be a cause of treatment-related mortality.[9]
The increased complexity of assessing treatment response and detecting adverse events led to the further development of RECIST 1.0 into irRC (immune-related response criteria) in 2009. The big news in irRC, derived from the new phenomenon of pseudoprogression (previously described), was the required confirmation of progression on two consecutive scans. It also included new lesion measurements in the entire tumor burden.[9]
After several consecutive implementations, irRC was further developed into the currently effective 2017 iRECIST standard, introduced in 2017. iRECIST included the concept of unconfirmed PD (iUPD) as a way to label tumors where treatment response is unclear and where a second scan in four to eight weeks is required to confirm PD, retain iUPD with a consecutive scan, or relabel as other treatment progression.[9]
Hence, the introduction of iRECIST for immune-oncology cases places additional demands on intuitive diagnostic tools such as marking, comparing, and keeping track of tumors on several consecutive scans made on different modalities on different time stamps. Integrated structured reporting templates that guide the radiologists will also facilitate the assessment of iRECIST.
The figure below demonstrates a case of appearance of new lesions after treatment initiation followed by treatment response. In this scenario, a RECIST 1.1 criteria would have classified this new lesion as disease progression and indicative of treatment failure. But the consecutive scan required in 2017 iRECIST confirms treatment response.[9]
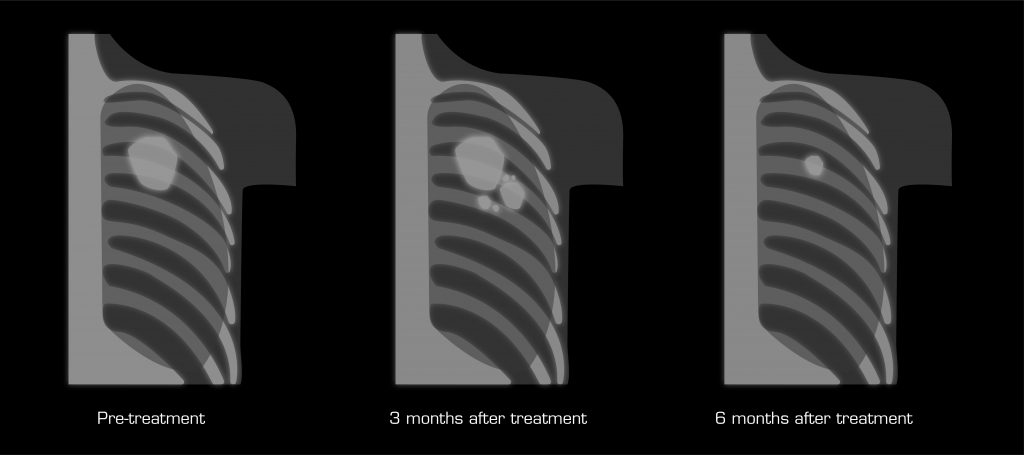
Figure 5. Illustration of the appearance of new lesions after treatment initiation.
When it comes to immunotherapy, a broad set of imaging techniques is used for detection, characterization, staging, therapeutic efficacy assessment, and recurrence and metastasis surveillance of various malignancies. Current research in the field is massive, ranging from traditional anatomical imaging to functional imaging, molecular imaging, and radiomics.
Within cancer imaging, anatomical imaging using CT and MRI is standard clinical practice, as it is in immune-oncology. For example, high‐resolution CT is frequently used for the screening of single pulmonary nodules, whereas contrast‐enhanced MRI is usually applied to detect brain metastases.[10] Other modalities can provide additional information necessary for assessing treatment response.
Functional imaging provides additional information regarding the tumors’ biological behaviors and can refine diagnostic, prognostic and predictive biomarkers[11]. For instance, dynamic contrast‐enhanced MRI (DCE‐MRI) can be used to investigate the relationship between tumor microvascularity and histopathological grade, the tendency towards metastasis and recurrence, patient prognosis, etc[10].
In addition, diffusion‐weighted imaging (DWI) can be applied to characterize tumors and identify early changes under treatment. DWI permits the measurement of random translational diffusion of water molecules and therefore provides additional pivotal information. For example, apparent diffusion coefficient (ADC), a quantitative parameter derived from DWI, can reveal the magnitude of water molecule motion in the extracellular compartment. This is of value since malignancies may demonstrate restricted diffusion (lower ADC values) because of their high cellularity, whereas tumors with increased diffusion (higher ADC values) can be seen as evidence of treatment response. This can be explained by the inflammation and necrosis caused by effective treatment, characterized by water retention and decreased cellularity.[10] A reduced ADC value of the tumor lesions might also be a sign of delayed response to treatment due to the infiltration of inflammatory cells[12].
The suboptimal image quality and low reproducibility of ADC measurements may hinder the applicability of DWI in practice. Therefore, it is recommended that diffusion images be interpreted in conjunction with conventional MRI sequences (such as T1WI, T2WI, and contrast‐enhanced sequences).[12]
Furthermore, 18F‐fluorodeoxyglucose (18F‐FDG) PET provides complementary information to anatomical imaging by detecting tumor metabolic changes, which is generally used for the diagnosis and staging of tumors with aggressiveness.[10]
An 18F‐FDG PET/CT scan can depict early changes in tumor metabolism prior to obvious morphologic changes (seen in anatomical imaging) that can be used to predict treatment efficacy. However, despite the fact that outcomes from several studies[13–16] indicated that 18F‐FDG PET/CT scans can provide valuable complementary information to traditional anatomical imaging, it has its drawbacks as 18F‐FDG uptake is not specific for tumors. Other processes, including inflammatory reaction, can also show elevated glucose metabolism, which poses a significant challenge for radiologists when it comes to distinguishing tumor progression from inflammation on PET scans.[17]
Molecular imaging is a subset of functional imaging that has enormous potential to produce a large number of biomarkers. The application of molecular imaging is related to employing radiolabeled antibodies, antibody fragments, peptides, and proteins to track immune checkpoint targets at the cellular and molecular levels to uncover the dynamic changes of the biomarkers’ expression.[18]
Currently, effective efforts are underway to define PD‐L1 or PD‐1 expression using non-invasive molecular probes[10]. This means a visualization of PD‐L1 expression without the need for biopsy, which compared with an immunohistochemical technique can enable longitudinal monitoring of PD‐L1 status and reduce missed diagnoses due to small biopsy samples by assessing the level of PD‐L1 throughout body.[19] This is just one example on how molecular imaging can be used to predict treatment response.
Radiomics is an imaging processing and analysis technique that enables the conversion of radiology images into quantitative data and the subsequent mining of high‐dimensional data[10]. The goal of radiomics is to generate imaging‐based biomarkers to improve knowledge of tumor biological behaviors and advance the development of precision medicine.
Several studies have demonstrated that CT‐based radiomics features might effectively predict responses and prognosis in patients treated with immunotherapies[20–22]. However, certain barriers, including the image acquisition variability, the high probability of false‐positive results, overfitting, challenges in result interpretation and low reproducibility, are slowing down its clinical use.[23]
Integrated diagnostics, the integration of radiomic features into clinical, histopathological and genomic biomarkers, might provide added information regarding more precise malignant biological property profiling for predictive purposes. It might also assist in identifying and distinguishing between hyperprogression and pseudoprogression[24], one of the previously mentioned challenge.
Anatomical imaging, as the name suggests, shows the structure and physical form of tissues/organs but not their disease state. Detecting an abnormality involves identifying anatomical changes—usually this means advanced disease, not early disease.
Functional imaging refers to how a tissue/organ is “working”, meaning its physiological or biological state. There are many types of functional imaging, one of them is molecular imaging (i.e. it is a subset). Molecular imaging is the imaging of molecular signatures (targets, proteins, receptors, etc.) that are indicative of a disease state.
Molecular imaging is important because anatomical imaging may appear normal, yet disease may still be present.
Thanks to Chris Behrenbruch (PhD) for this explanation.
A lot of research is still going on within immunotherapy, and the assessment criteria such as iRECIST will continue to develop and diagnostic techniques will keep adding to the radiologist’s toolbox. Anatomical, functional, and molecular imaging techniques and radiomics will all be used together, creating high demands on diagnostic tools. Especially molecular imaging using novel radioactive tracers that target the key molecules of immune-checkpoint pathways and cellular immune responses will play a significant role in the future of immune-oncology.
Moreover, the use of radiomics will most likely play a key role, aiming to quantify imaging features and link them to clinically relevant parameters such as tumor subtype, patient prognosis, and therapy outcome prediction[25].
Being on the cutting edge of these techniques and having access to the right tools in the diagnostic workstation, such as integrated standard templates supporting iRECIST, efficient volume measurement tools, and functions for labeling, measuring size, and following tumor progression over time, will be a prerequisite for being able to master the rapid development within immunotherapies.
Revision date: January 26, 2021