Automation, AI, and other imminent trends
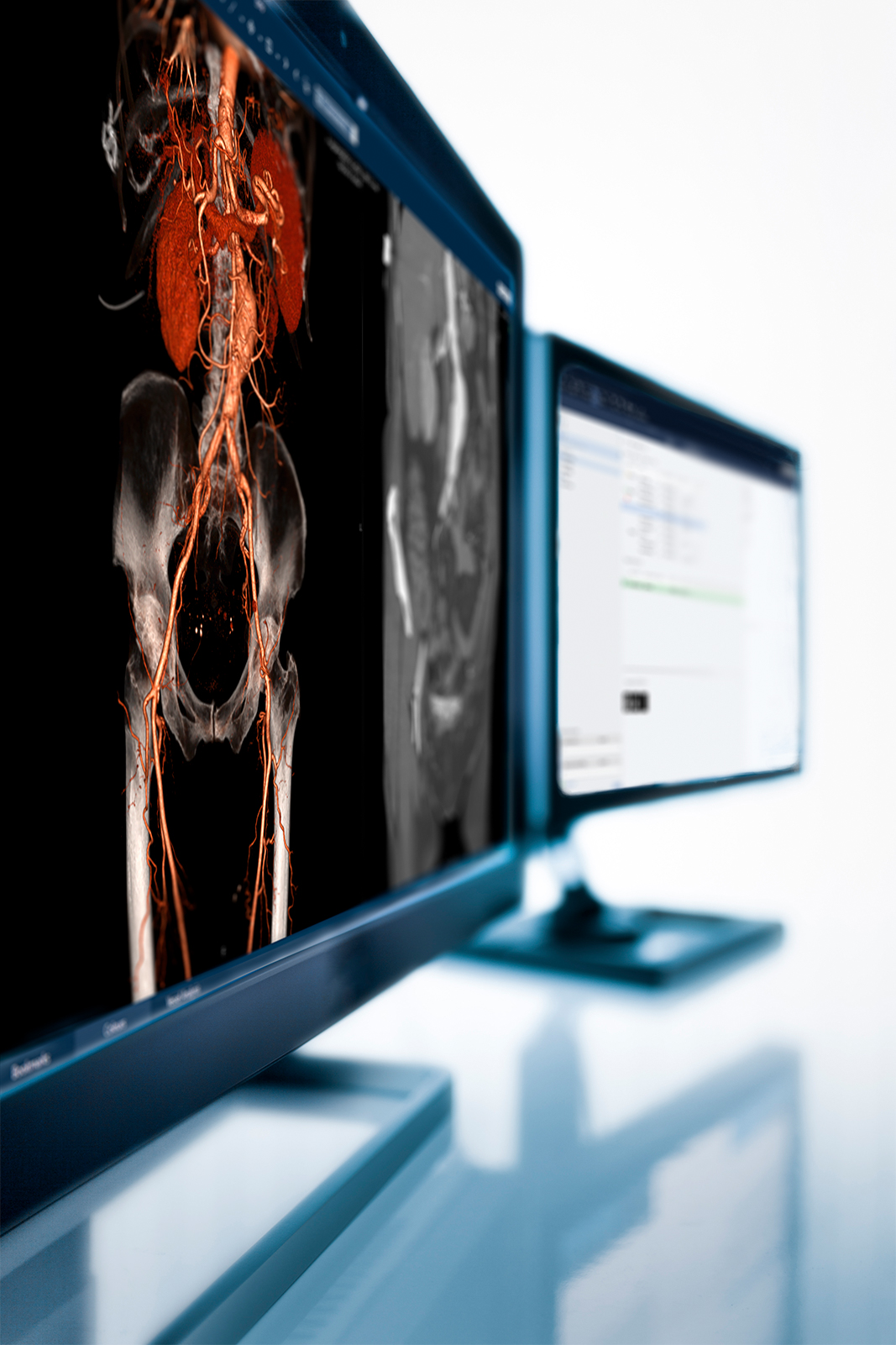
Continuing the topic of automation, Dr. Newton explains where he believes things are heading. “Here at East Lancashire, we’ve implemented automatic lung nodule detection that detects on the previous scan, and on the current scan it tells you the volume doubling time. It allows you to quickly conclude whether a lung nodule is benign or not. So, we’ve already got the first example of what I talked about just before. But this kind of solution needs to spread to the rest of the body, picking up bone metastasis instantly, and comparing to previous scans to speed up your reporting times. But it could do the same thing for adrenal nodules, liver lesions, nodes, pelvis, etc. A lot of that could be automated, and I think that is the way things are going.”
“I also believe the vetting process has potential to be automated to a large extent,” he continues. “I don’t know whether this is the same in other countries, but here in the UK, when we get a request through, we have to vet it and make sure that the right protocol is assigned to it, make sure whether or not to give contrast. A lot of that could be automated, and if it was, that work could be devolved to the radiographers. I probably spend three quarters of an hour per day vetting when I do clinical work, vetting the scans—if all that was automated, that would save me a lot of time.”
“Here in Leiden, we actually apply AI at multiple levels already—on image acquisition, on image interpretation, but also on the workflow,” Prof. van Buchem describes. “On the acquisition side, we’re actively working on a project where we use AI to speed up MR acquisitions. One of the limiting factors in the workflow in our department is the duration of the scan time for the MR—if we can speed that up, it will reduce the cost per scan and increase our capacity. So far, it looks very promising—speeding up MR acquisitions by up to four to eight times. We’re now expanding this project from knees, where we started, into other body parts.”
He continues, “In the image interpretation phase, there are a number of techniques that we also use for automatic analysis of the data, of the scans. But I also expect a lot from AI in the workflow. Patient scheduling is a good example where I believe AI will add value. For example, we’ve seen interesting data from a group in Sweden; we always think, in an ideal world, that a time slot for a given examination should be entirely determined by the length of the sequences that you use, in the MR scenario. But they have shown that there’s a wide variation in the time it takes for a time slot for a given patient. For cooperative, young patients it can be shorter, but for an older or invalid patient it can take much longer time. By using AI, you can predict which patients need a certain amount of time for a given examination. That’s a good example of how AI could improve the radiology workflow.”
“To summarize,” Prof. van Buchem says, “AI is not just for image interpretation—I mean, it’s great for that and it’s very important! Maybe less exciting, but at least as important, are AI applications in image acquisition on the one hand, and workflow on the other hand. Also, the easiest one to start with from a legal perspective is workflow. Because you don’t need all kinds of legislation and regulations to pass. There’s no need for that certification.”
“In regards to AI, what we do here in Bergen is a lot of research, especially within mammography screening, to validate that new AI-based tools really do what they are supposed to do,” Prof. Dr. Aslaksen says. “In addition, what we’re also working on is developing research repositories and archives together with Sectra. And also using ‘AI as a service’ for the researchers to build a biobank, so to say, for research studies, so they don’t have to develop their own AI system, but can ask us to do the work for them as a service.”
“Another interesting trend that I would like to bring up,” he continues, “is the increasing collaboration between radiology and nuclear medicine: SPEC-CT, PET-CT, and we also have a PET-MR in our department, especially used for pelvis, prostate, and CNS imaging. The trend of increasing collaboration between oncologists, radiologists, and nuclear medicine physicians, both in diagnostic and therapeutic imaging, is something I think will accelerate in the future.”
Dr. Henriksson takes over and can’t hide his enthusiasm for the topic discussed. “An immensely fascinating subject—the amount of improvement potential in every workflow step that we do is immense, so we could easily talk about this for two days straight,” he says and laughs. “For me and my colleagues, one of the most important things to address is the need for deep workflow integration so that the mechanisms, be it machine learning or whatever, are integrated back-end and don’t come with additional buttons for us radiologists. Everything should be as automatic as possible, even though there are smart orchestration engines in the background that do a lot of magic for you—the radiologists don’t want to see it, they don’t want to choose on/off, they just want it configured in their worklists and as simple as possible. I think that is a significant driver of efficiency that has potential to help us help more patients per hour—combined with trust, of course. You need to know that it actually works.”
“And speaking of automation, one thing that I hope for, going forward, is that we can make the diagnostic system aware of our different competence profiles and link that to the different exams, so that we can automatically route the exams to the right competences or profiles—that would be a big win,” Dr. Henriksson continues. “I have 50 radiologists with very different profiles; some of them are very general, some are very deep in niched areas. Now, they are scrolling through these worklists trying to understand which exams are suitable for their respective competence, where they can create the most value.”
One additional aspect that both Dr. Henriksson and Dr. Newton agree is very time consuming is sifting through the patient history to find all the relevant priors—not least for patients with cancer who have sometimes undergone 30–50 exams in the past. “If there was some sort of automated tool, maybe using really basic AI just to work out to exactly what type of study it was, and then use that to retrieve the relevant studies, I think that would be a quick win,” Dr. Newton says.