The right conditions for a pilot test in Skåne
The solution that was developed is based on making all of the documentation related to MRI investigations, biopsies, and pathology reports structured and digital. Thanks to the digital structure, the information can be transferred directly to the medical record and to the prostate cancer registry if prostate cancer has been established. The working group saw several advantages with the solution in theory, but the integrated flow needed to be properly evaluated.
Region Skåne and Helsingborg Hospital came up as natural candidates for a pilot test in a clinical setting early on. For one thing, they had already been using parts of the solution, and they already had the right technical capabilities for integrated diagnostics in place. For another thing, the hospital was considered “the right size” to conduct a reasonable project.
The region has been a customer of Sectra’s for many years, and Sectra’s PACS has been used as a diagnostics application region-wide in both radiology and pathology. Before the pilot project, a close dialogue and partnership took place between the hospital in Helsingborg, the RCC and Sectra to address the working group’s requests, improve the existing functionality of the solution, and develop a function for automatic feedback from INCA that is integrated into Sectra PACS. Both Johan and Erik describe the partnership as “running extremely smoothly” and “invaluable.”
“In general, technical integrations tend to be complex and difficult, but I think things went smoothly here,” says Johan. “We had a constructive initial meeting attended by a Sectra solutions architect who immediately understood our needs and requirements and could bring them to product development. A technical concept was developed before the summer, and development took place during a few weeks in August, so we were able to install the solution in September.”
“The NPCR had a long list of requests before startup, and Sectra took the list and was able to implement it. It was wonderful when we got it to work—we were practically saying ‘hallelujah’ here,” Erik adds.
The vision of the pilot project, Johan continues, was to be able to test using the three structured report templates and the functions built into the templates in practice. “Of course we wanted to evaluate the result and what the professionals concerned—radiologists, urologists, and pathologists, as well as medical secretaries, nurses, biomedical analysts, and others who file reports in the quality registry—thought about the work method and the flow. We wanted to get the operational work method up and running properly and without too much fuss, then provide the users with a thorough introduction and develop practical work processes and procedures together.”
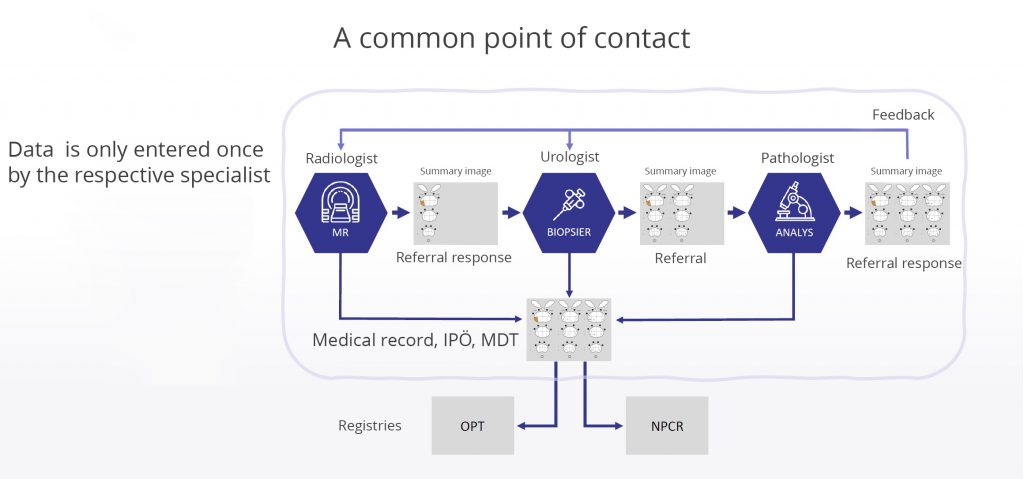
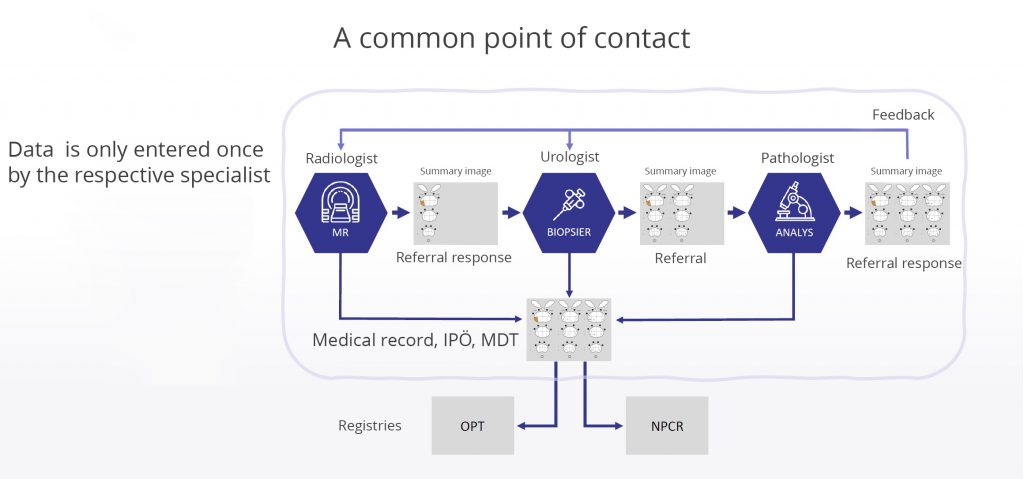
Overview of the diagnostic chain with a feedback loop. A single-entry model, consisting of the initial documentation by each physician, is sufficient for creating referral replies, graphic visualization in the interactive decision support tool Individual Patient Overview for prostate patients, and registration in the NPCR. Image: NPCR
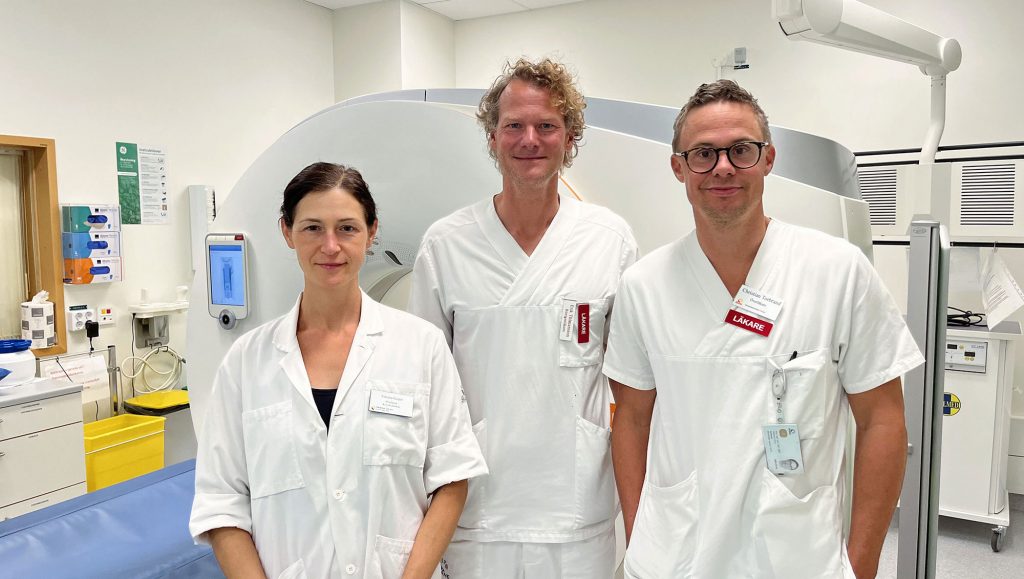
The pilot test ran from early September 2023 until December 1. It included around 100 biopsy patients, and around 50 staff members at Helsingborg Hospital participated in the pilot, Erik explains. “At the hospital, I’m the person in charge of the radiology part; senior physician Viktoria Gaspar is in charge of the pathology part; and senior physician Christian Torbrand is in charge of urology. Here in Helsingborg, we have ten radiologists who write prostate MRI reports, and all of them participated. Aside from us, the pilot involved a handful of pathologists, several urologists, and several nurses in all three units that participated.”
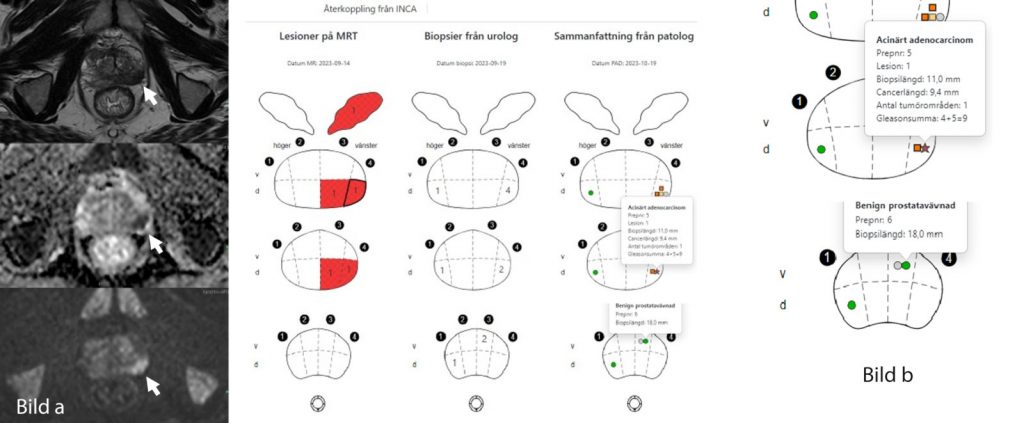
Erik explains that the radiologists in Helsingborg, who review a handful of prostate cases per week on average, changed very little in their workflow; they were able to work as usual and submit reports using the review template in Sectra PACS, which is automatically synchronized with the quality registry. Automatic feedback from INCA was an additional feature that was activated for them during the pilot. As soon as the pathology opinion is completed, each radiologist receives feedback on their cases in an individual dynamic work list in PACS. This might seem like a small change, but it is extremely important to the radiologists, and Erik and his colleagues found it unbelievably valuable.
“It’s important to us to find out where the biopsies were taken and what they showed,” Erik says. “When we wanted to follow up on a case in the past, we either had to log in to the patient’s medical records and search, which is time-consuming, or if we were lucky, the case came up at a multidisciplinary team meeting, which does not happen for many cases. The great thing about the built-in feedback from INCA is that we now receive a summary from the urologist and pathologist directly in our diagnostic tool via a so-called web window. The feedback thus becomes individualized and automated—an unbelievably seamless solution, which is extremely valuable. Naturally, it’s good to know if I was right, but perhaps it’s even more important to find out when my assessment was incorrect. By having this feedback loop, we build on our personal experience and can calibrate ourselves and become better radiologists over time. We can also reduce what we call overdiagnosis and avoid saying that cancer is present when there actually isn’t any cancer.”