References
Azzato EM, Morrissette JJD, Halbiger RD, Bagg A, Daber RD (2014). Development and implementation of a custom integrated database with dashboards to assist with hematopathology specimen triage and traffic. J Pathol Inform 5(1):29.
Baidoshvili A, Bucur A, van Leeuwen J, van der Laak J, Kluin P, van Diest PJ (2018). Evaluating the benefits of digital pathology implementation: time savings in laboratory logistics. Histopathol 73(5):784-794.
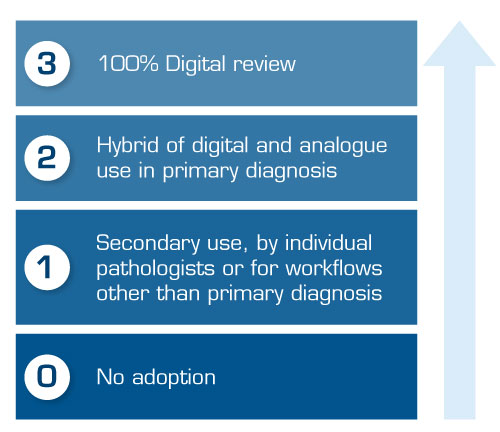
Griffin J, Treanor D (2017). Digital pathology in clinical use: where are we now and what is holding us back? Histopathol 70(1):134-145.
Hanna MG, Reuter VE, Samboy J, England C, Corsale L, Fine SW, Agaram NP, Stamelos E, Yagi Y, Hameed M, Klimstra DS, Sirintrapun SJ (2019). Implementation of Digital Pathology Offers Clinical and Operational Increase in Efficiency and Cost Savings. Arch Pathol Lab Med 143(12):1545-1555.
Häger S (2016). How to build a business case to justify the investment in digital pathology. https://medical.sectra.com/ resources/how-to-build-a-business-case-to-justify-the-investment-in-digital-pathology/.
Ho J, Ahlers SM, Stratman C, Aridor O, Pantanowitz L, Fine JL, Kuzmishin JA, Montalto MC, Parwani AV (2014). Can Digital Pathology Result In Cost Savings? A Financial Projection For Digital Pathology Implementation At A Large Integrated Health Care Organization. J Pathol Inform 5(1):33.
KLAS (2019), Digital pathology 2019: What you need to get started, Utah: Klas Research.
Nakhleh RE, Zarbo RJ (1996). Surgical pathology specimen identification and accessioning: A College of American Pathologists Q-Probes Study of 1 004 115 cases from 417 institutions. Arch Pathol Lab Med 120(3):227-33.
Nakhleh RE, Idowu MO, Souers RJ, Meier FA, Bekeris LG (2011). Mislabeling of cases, specimens, blocks, and slides: a college of american pathologists study of 136 institutions. Arch Pathol Lab Med 135(8):969-74.
Pantanowitz L (2016). A Business Case for Common Sense. The Pathologist. https://thepathologist.com/outside-thelab/ a-business-case-for-common-sense.
Sandeman K, Bauer T (2020). Digital pathology for routine diagnostics — experiences from Region Skåne & Hospital for Special Surgery. The Pathologist. https://thepathologist.com/webinar/digital-pathology-for-routine-diagnosticsexperiences- from-region-skaane-hospital-for-special-surgery.
Stathonikos N, Nguyen TQ, Spoto CP, Verdaasdonk MAM, van Diest PJ (2019). Being fully digital: perspective of a Dutch academic pathology laboratory. Histopathol 75(5):621–635.
Stratman C (2011). Digital Pathology in the Clinical Workflow: A Time & Motion. Pathology Visions. Oral presentation.
Vodovnik A (2016). Diagnostic time in digital pathology: A comparative study on 400 cases. J Pathol Inform Jan 29;7:4.
Williams BJ, Bottoms D, Clark D, Treanor D (2019). Future-proofing pathology part 2: building a business case for digital pathology. J Clin Pathol 72(3):198-205.